How Trauma Changes the Brain and Body
The neuroscience explains how trauma changes the brain and body, and why distressing experiences leave lasting imprints, disrupting emotional regulation, memory, and stress responses. Trauma rewires the brain and body, impacting fear and emotions. Trauma is not just a psychological struggle—it is a neurobiological condition rooted in structural and functional changes to the brain. These changes affect cognition, behavior, and physiological states, often trapping individuals in cycles of fear and hyperarousal. Understanding how trauma changes the brain and body provides insight into how evidence-based treatments like Cognitive Behavioral Therapy (CBT) and Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)can help restore balance and regain control.
How Trauma Rewires the Brain
How trauma changes the brain and body leads to significant changes in three key brain regions involved in fear processing, memory, and emotional regulation:
- Amygdala: The brain’s fear center becomes hyperactive, heightening threat perception and causing individuals to feel constantly on edge. Everyday stimuli can trigger intense fear responses, even in safe environments.
- Hippocampus: Responsible for memory formation and distinguishing past from present, the hippocampus often shrinks after trauma. This reduction contributes to intrusive memories, flashbacks, and difficulty differentiating between real and perceived threats.
- Prefrontal Cortex: This region, which regulates emotions and rational thinking, becomes underactive. Impaired function reduces an individual’s ability to regulate fear responses, making them more reactive and less able to counteract emotional distress.
Together, these changes explain why trauma symptoms persist and can be difficult to control. The overactive amygdala and underactive prefrontal cortex create an imbalance that reinforces hypervigilance, intrusive thoughts, and emotional dysregulation.
When Trauma Becomes PTSD
Experiencing trauma does not always lead to Post-Traumatic Stress Disorder (PTSD), but for some, the brain’s response to distressing events becomes deeply ingrained. Trauma can overwhelm the nervous system, but most people gradually recover. PTSD develops when the brain remains stuck in a heightened state of fear and stress, leading to persistent symptoms.
People with PTSD often experience flashbacks, which are vivid, involuntary re-experiences of the trauma, making them feel as if they are reliving it. Other symptoms include avoidance of reminders, emotional numbness, and hypervigilance. These arise from brain changes, including an overactive amygdala (fear processing) and an underactive prefrontal cortex (emotional regulation).
The Body’s Response to Trauma
Trauma profoundly impacts the body through the autonomic nervous system (ANS), which controls involuntary functions like heart rate and digestion. Trauma can dysregulate the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), leaving individuals stuck in a state of hyperarousal or dissociation.
Hyperarousal: The Fight-or-Flight Response
When the SNS is overactive, individuals experience:
- Increased heart rate and blood pressure
- Shallow breathing
- Muscle tension and restlessness
- Difficulty sleeping
- Exaggerated startle response
This constant state of alertness is exhausting and can contribute to secondary conditions like chronic pain, gastrointestinal issues, and autoimmune disorders.
Dissociation: The Freeze Response
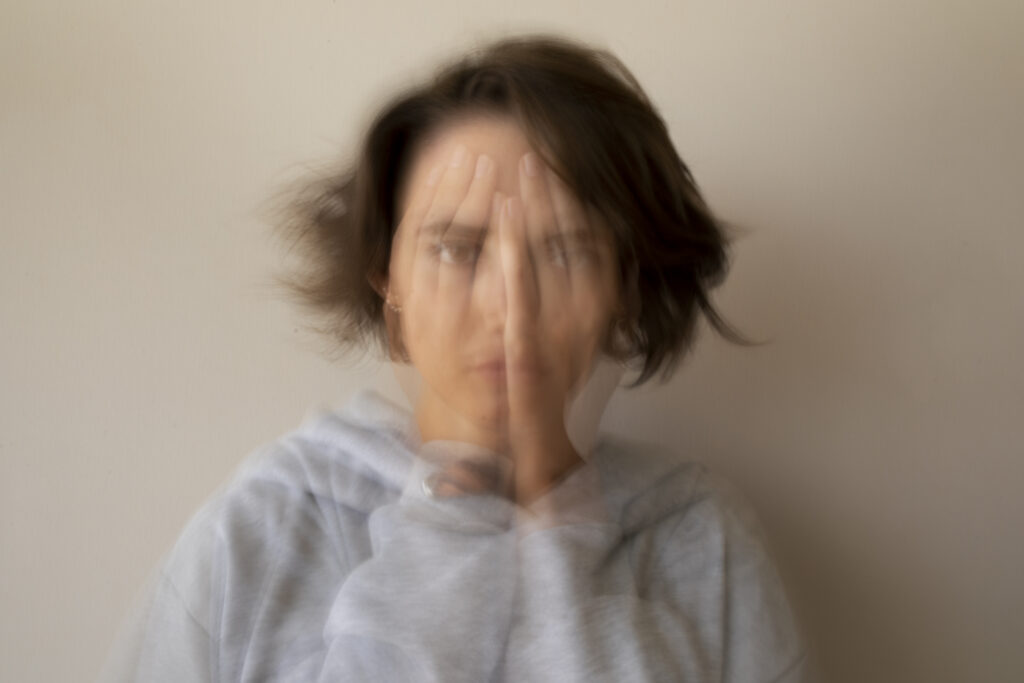
Alternatively, some individuals experience dissociation, a coping mechanism where the body shuts down in response to overwhelming stress. Symptoms include:
- Emotional numbness
- Memory gaps (dissociative amnesia)
- Feeling disconnected from reality (depersonalization)
- Fatigue and low energy
Understanding Dissociation
What is Dissociation?
Dissociation is a mental process where a person disconnects from their thoughts, feelings, memories, or sense of identity. It can manifest in various ways, such as identity confusion, intrusive thoughts, flashbacks, depersonalization, and derealization. During traumatic experiences, dissociation can serve as a survival mechanism, allowing individuals to mentally escape overwhelming situations.
Why Do People Dissociate During Trauma?
Dissociation is often triggered during trauma as an automatic response to extreme fear or helplessness. When a person perceives imminent danger, their nervous system activates a defense mechanism known as the defense cascade, which includes freeze, flight, fight, fright, flag, and faint responses. Dissociation is most likely to occur during the latter stages, when the body enters a state of immobilization and emotional numbing to cope with inescapable danger.
Long-Term Effects of Dissociation
Individuals who have experienced dissociation during trauma may continue to experience its effects long after the event. These may include:
- Flashbacks and Intrusive Memories: Vivid recollections of the traumatic event that feel as if they are happening in the present.
- Emotional Numbing: A lack of emotional responsiveness or a sense of detachment from reality.
- Feeling Disconnected from Reality: A sensation of being spaced out or dissociated from one’s surroundings.
Managing Dissociation with Grounding Techniques
Grounding techniques help individuals reconnect with the present moment and regain control over dissociative symptoms. These techniques fall into two main categories:
1. Sensory Grounding Techniques
These techniques use the five senses to anchor a person to their surroundings:
- Sight: Identify five things you can see around you.
- Sound: Focus on specific sounds, such as birds chirping or a ticking clock.
- Touch: Hold a textured object, such as a stone or piece of fabric, to bring awareness to your body.
- Smell: Use a strong scent, such as peppermint or lavender, to reconnect with reality.
- Taste: Suck on a mint or take a sip of a flavored drink to engage your sense of taste.
2. Cognitive Grounding Techniques
These techniques use mental exercises to focus on the present:
- Orient Yourself: State your name, the date, and where you are to reinforce awareness.
- Self-Reassurance: Repeat comforting phrases such as “I am safe now” or “This moment is different from my past.”
- Mindfulness: Focus on deep breathing or guided meditation to bring awareness to the present.
Integrating Neuroscience into Trauma Recovery
Healing from trauma requires a comprehensive, evidence-based approach that combines both top-down (thouth process) and bottom-up (body sensations) therapies. Cognitive interventions like CBT and TF-CBT help reframe thought patterns, while mindfulness, exercise, and grounding techniques work to restore physiological balance.
By understanding how trauma changes the brain and body, we can develop effective, individualized treatment plans that empower individuals to regain control. Whether through therapy, medication, or physiological interventions, the ultimate goal is to restore a sense of safety, resilience, and well-being.
If you’re ready to begin your healing journey and take back control, reach out here to schedule a consultation and explore how therapy can support your recovery.

Hi! I’m a psychologist and the founder of Intercultural Psychology in Dublin, specializing in psychotherapy and CBT. I work with individuals from diverse cultural backgrounds and neurodiverse clients, helping them navigate life’s challenges, adjust to new environments, and grow along the way. I hope this blog encourages you to embrace your journey and inspires positive change in your life :).